EMS.gov | New Resources Address Important EMS Issues
|
|
|
|
|
|
|
|
Jonathon Feit eulogizes Mike Touchstone for making significant contributions to advance EMS and fire leadership.
|
|
|
|
|
|
Heroes who look past danger to help people in need,
Heroes to step in to be the difference between triumph and tragedy,
And Heroes who use their minds to create technology that saves lives.
We need those Heroes.
GoAERO is offering $2+ Million in prizes for the best thinkers, creators and inventors to build Emergency Response Flyers and stretch and challenge their minds to unlock a new era of disaster and rescue response.
By unleashing the power of autonomy, speed, and precision, GoAERO is looking for the brightest, boldest and bravest to change the way we rescue and respond to disaster.
This is your chance to make history and save lives.
From the Centers for Medicare & Medicaid Services on March 9
The Centers for Medicare & Medicaid Services (CMS) is continuing to monitor and assess the impact that the cyberattack on UnitedHealth Group’s subsidiary Change Healthcare has had on all provider and supplier types. Today, CMS is announcing that, in addition to considering applications for accelerated payments for Medicare Part A providers, we will also be considering applications for advance payments for Part B suppliers.
Over the last few days, we have continued to meet with health plans, providers and suppliers to hear about their most pressing concerns. As announced previously, we have directed our Medicare Administrative Contractors (MACs) to expedite actions needed for providers and suppliers to change the clearinghouse they use and to accept paper claims if providers need to use that method. We will continue to respond to provider and supplier inquiries regarding MAC processes.
CMS also recognizes that many Medicaid providers are deeply affected by the impact of the cyberattack. We are continuing to work closely with States and are urging Medicaid managed care plans to make prospective payments to impacted providers, as well.
All MACs will provide public information on how to submit a request for a Medicare accelerated or advance payment on their websites as early as today, Saturday, March 9.
CMS looks forward to continuing to support the provider community during this difficult situation. All affected providers should reach out to health plans and other payers for assistance with the disruption. CMS has encouraged Medicare Advantage (MA) organizations to offer advance funding to providers affected by this cyberattack. The rules governing CMS’s payments to MA organizations and Part D sponsors remain unchanged. Please note that nothing in this statement speaks to the arrangements between MA organizations or Part D sponsors and their contracted providers or facilities.
For more information view the Fact Sheet: https://www.cms.gov/newsroom/fact-sheets/change-healthcare/optum-payment-disruption-chopd-accelerated-payments-part-providers-and-advance
###
Heroes who look past danger to help people in need,
Heroes to step in to be the difference between triumph and tragedy,
And Heroes who use their minds to create technology that saves lives.
We need those Heroes.
GoAERO is offering $2+ Million in prizes for the best thinkers, creators and inventors to build Emergency Response Flyers and stretch and challenge their minds to unlock a new era of disaster and rescue response.
By unleashing the power of autonomy, speed, and precision, GoAERO is looking for the brightest, boldest and bravest to change the way we rescue and respond to disaster.
This is your chance to make history and save lives.
|
In the ever-evolving landscape of workforce management, Ninth Brain emerges as a pioneering force, dedicated to delivering innovative solutions that prioritize cutting-edge technology, user-friendly features, and steadfast compliance.
As Ninth Brain continues its journey, they are thrilled to unveil insights into key functionalities that position them as a leader in the industry.
Developer Open API: Seamless Integration
Central to Ninth Brain’s commitment to seamless data integration is their Developer Open API. Features like the Forms Module API Endpoint enables management to effortlessly retrieve form responses, facilitate in-depth analysis and examine with external dashboard utilization. The Run Log Module API Endpoint empowers management to monitor and analyze debriefs, chart reviews, and utilization responses, providing invaluable insights into its patient care.
OSHA Logs and Electronic Reporting: Simplified Compliance
In the realm of Emergency Medical Services, compliance with OSHA regulations is paramount. Ninth Brain’s Employee Health module streamlines the management of workplace injuries, illnesses, and incidents. This not only ensures compliance but also enhances reporting efficiency, enabling EMS agencies to focus on their life-saving missions.
Captain Grey Matter/Co-Owner, Lisa Tedford, underscores the commitment: “Our team is dedicated to researching regulations and finding innovative ways to enhance our platform. We aim to alleviate tasks for busy administrators, making our partners more efficient and ensuring ongoing compliance. The recent update to the Employee Health module was driven by the need to keep agencies compliant with the new 2024 electronic reporting mandate, designed to simplify the submission process.”
Single Sign-On: Effortless Access
Ninth Brain’s adoption of Single Sign-On (SSO) has revolutionized the user experience, providing a simplified and secure login process. Centralizing authentication, SSO reduces password fatigue, enhances security, and streamlines administrative management. Password Administrators are encouraged to explore the benefits of SSO with their tech teams, as enabling this feature is an impactful and positive change.
Accreditation Assistant: Streamlined Process
Notably, Ninth Brain recently introduced the Accreditation Assistant, revolutionizing the compliance journey for EMS leaders with features tailored for accreditation and reaccreditation, streamlined processes, and intelligent recommendations, reinforcing Ninth Brain’s commitment to comprehensive solutions.
Co-Owner Holly Taylor emphasizes, “At Ninth Brain, we’re all about making things better. Our latest software enhancements? They’re like your personal efficiency boosters, helping our partners get things done smarter and keeping them in the compliance sweet spot. We’re not just here to deliver software; we’re here to make their work life a whole lot easier!”
By highlighting these features, Ninth Brain reaffirms its commitment to supporting EMS agencies in optimizing workforce management, ensuring compliance, and contributing to the successful delivery of life-saving services. As they look ahead, Ninth Brain remains at the forefront of industry compliance, continuously enhancing its software to meet the evolving needs of its clients.
About Ninth Brain: Ninth Brain’s mission is to be a long-standing partner with First Responder agencies by providing quality and intuitive software solutions that evolve with the industry. They bundle comprehensive software with a fun, devoted, and knowledgeable support team that make their clients their top priority. Throughout the past 20+ years of their journey, Ninth Brain has continuously developed enhancements to provide efficiencies, aid in industry compliance, and ultimately elevate patient care practices. Ninth Brain offers Credential Tracking, Learning Management System, Workforce Scheduling, Quality Improvement Tracking, Digital Forms and Checklists, and more! To learn more, visit www.ninthbrain.com
Contact: Holly Taylor, Chief Hat Holder
Phone: 888-364-9995 ext. 320
Email: Holly@ninthbrain.com
AAA President Randy Strozyk will testify tomorrow, February 14, at 10:00 am (eastern) before the Health Subcommittee of the Energy and Commerce Committee of the U.S. House of Representatives. The hearing is on “Legislative Proposals To Support Patients And Caregivers” and Randy will speak to the SIREN Reauthorization Act (H.R. 4646), EMS for Children Reauthorization Act (H.R. 6960) and legislation to reauthorize the Traumatic Brain Injury program (H.R. 7208) and certain poison control programs (H.R. 7251).
The hearing will be live streamed online at https://youtu.be/Zy-4NCuheGM.
The hearing will provide the AAA and Randy with a platform to voice support for the EMS proposals on the agenda as well as raise the need for the Committee to address our Medicare ambulance add-on payments and the EMS workforce shortage. For a copy of Randy’s written testimony and other details of the hearing, please go to the Committee website for the hearing.
From the Journal of Emergency Medical Services on February 1, 2024
Why are females and individuals who identify as Black, indigenous and/or People of Color underrepresented in EMS?
The U.S. Department of Health and Human Services Office of the Administration for Strategic Preparedness and Response (ASPR) and Project ECHO have launched this program designed to create peer-to-peer learning networks where clinicians who have more experience treating patients in emergency situations share their challenges and successes with clinicians across the U.S. and around the world with a wide variety of experience of these situations. Topics for sessions are based on new and emergent information around emergency preparedness, as well as topics requested by participants.
Sessions will be eligible for CME credits.
Please contact C19ECHO@salud.unm.edu for more information.
From EMS.gov on January 24, 2024
|
|
|
|
Air Evac Lifeteam is heartbroken to report that three crew members have perished in an incident that occurred on Saturday, January 20. At 11:23 pm local time AEL’s Operations Control Center (OCC) lost contact with the aircraft, a Bell 206L3 with call sign N295AE. The crew is based out of Weatherford, OK, and was returning to base after completing a patient care transport in Oklahoma City when the OCC lost contact with them. Nearby AEL teams assisted local law enforcement with the search.
Our primary focus is on supporting the families and our team members. CISM teams have been sent to assist our team members during this time.
It is with a heavy heart that we share the names of our three colleagues. Pilot Russell Haslam, Flight Nurse Adam Tebben and Flight Paramedic Steven Fitzgerald. We continue to hold their families in our hearts.
AEL has turned over the scene and investigation to the NTSB
Final rule modernizes the health care system and reduces patient and provider burden by streamlining the prior authorization process
As part of the Biden-Harris Administration’s ongoing commitment to increasing health data exchange and strengthening access to care, the Centers for Medicare & Medicaid Services (CMS) finalized the CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F) today. The rule sets requirements for Medicare Advantage (MA) organizations, Medicaid and the Children’s Health Insurance Program (CHIP) fee-for-service (FFS) programs, Medicaid managed care plans, CHIP managed care entities, and issuers of Qualified Health Plans (QHPs) offered on the Federally-Facilitated Exchanges (FFEs), (collectively “impacted payers”), to improve the electronic exchange of health information and prior authorization processes for medical items and services. Together, these policies will improve prior authorization processes and reduce burden on patients, providers, and payers, resulting in approximately $15 billion of estimated savings over ten years.
“When a doctor says a patient needs a procedure, it is essential that it happens in a timely manner,” said HHS Secretary Xavier Becerra. “Too many Americans are left in limbo, waiting for approval from their insurance company. Today the Biden-Harris Administration is announcing strong action that will shorten these wait times by streamlining and better digitizing the approval process.”
“CMS is committed to breaking down barriers in the health care system to make it easier for doctors and nurses to provide the care that people need to stay healthy,” said CMS Administrator Chiquita Brooks-LaSure. “Increasing efficiency and enabling health care data to flow freely and securely between patients, providers, and payers and streamlining prior authorization processes supports better health outcomes and a better health care experience for all.”
While prior authorization can help ensure medical care is necessary and appropriate, it can sometimes be an obstacle to necessary patient care when providers must navigate complex and widely varying payer requirements or face long waits for prior authorization decisions. This final rule establishes requirements for certain payers to streamline the prior authorization process and complements the Medicare Advantage requirements finalized in the Contract Year (CY) 2024 MA and Part D final rule, which add continuity of care requirements and reduce disruptions for beneficiaries. Beginning primarily in 2026, impacted payers (not including QHP issuers on the FFEs) will be required to send prior authorization decisions within 72 hours for expedited (i.e., urgent) requests and seven calendar days for standard (i.e., non-urgent) requests for medical items and services. For some payers, this new timeframe for standard requests cuts current decision timeframes in half. The rule also requires all impacted payers to include a specific reason for denying a prior authorization request, which will help facilitate resubmission of the request or an appeal when needed. Finally, impacted payers will be required to publicly report prior authorization metrics, similar to the metrics Medicare FFS already makes available.
The rule also requires impacted payers to implement a Health Level 7 (HL7®) Fast Healthcare Interoperability Resources (FHIR®) Prior Authorization application programming interface (API), which can be used to facilitate a more efficient electronic prior authorization process between providers and payers by automating the end-to-end prior authorization process. Medicare FFS has already implemented an electronic prior authorization API, demonstrating the efficiencies other payers could realize by implementing such an API. Together, these new requirements for the prior authorization process will reduce administrative burden on the healthcare workforce, empower clinicians to spend more time providing direct care to their patients, and prevent avoidable delays in care for patients.
In response to feedback received on multiple rules and extensive stakeholder outreach HHS will be announcing the use of enforcement discretion for the Health Insurance Portability and Accountability Act of 1996 (HIPAA) X12 278 prior authorization transaction standard to further promote efficiency in the prior authorization process. Covered entities that implement an all-FHIR-based Prior Authorization API pursuant to the CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F) who do not use the X12 278 standard as part of their API implementation will not be enforced against under HIPAA Administrative Simplification, thus allowing limited flexibility for covered entities to use a FHIR-only or FHIR and X12 combination API to meet the requirements of the CMS Interoperability and Prior Authorization final rule. Covered entities may also choose to make available an X12-only prior authorization transaction. HHS will continue to evaluate the HIPAA prior authorization transaction standards for future rulemaking.
CMS is also finalizing API requirements to increase health data exchange and foster a more efficient health care system for all. CMS values public input and considered the comments submitted by the public, including patients, providers, and payers, in finalizing the rule. Informed by these public comments, CMS is delaying the dates for compliance with the API policies from generally January 1, 2026, to January 1, 2027. In addition to the Prior Authorization API, beginning January 2027, impacted payers will be required to expand their current Patient Access API to include information about prior authorizations and to implement a Provider Access API that providers can use to retrieve their patients’ claims, encounter, clinical, and prior authorization data. Also informed by public comments on previous payer-to-payer data exchange policies, we are requiring impacted payers to exchange, with a patient’s permission, most of those same data using a Payer-to-Payer FHIR API when a patient moves between payers or has multiple concurrent payers.
Finally, the rule also adds a new Electronic Prior Authorization measure for eligible clinicians under the Merit-based Incentive Payment System (MIPS) Promoting Interoperability performance category and eligible hospitals and critical access hospitals (CAHs) in the Medicare Promoting Interoperability Program to report their use of payers’ Prior Authorization APIs to submit an electronic prior authorization request. Together, these policies will help to create a more efficient prior authorization process and support better access to health information and timely, high-quality care.
The final rule is available to review here: https://www.cms.gov/files/document/cms-0057-f.pdf.
The fact sheet for this final rule is available here: https://www.cms.gov/newsroom/fact-sheets/cms-interoperability-and-prior-authorization-final-rule-cms-0057-f.
###
January 17, 2024 – Irving, TX We didn’t need emergency warning devices to get where we were going – a motor vehicle crash without serious injuries. We tried to change lanes and were hit from behind, sideswiped, and pushed across the road. We expected people to yield to us, but the bright flashing lights and sirens contributed to distracting the driver of the car as he was trying to get around us. I still to this day believe we wouldn’t have gotten crashed if we were driving without the use of the emergency warning devices.
The reality is when lights and sirens are on, the risk of crash increases by over 50%. Weekly, we hear reports of ambulance crashes that impact providers, patients, and the public.
The National EMS Quality Alliance has released Improving Safety in EMS: Reducing the Use of Lights and Siren, a change package with the results, lessons learned, and change strategies developed during the 15-month long Lights and Siren Collaborative. It will assist EMS organization in making incremental improvements to use of lights and siren on a local and systematic basis. “The best practices that have emerged from this project will allow every agency, regardless of service model or size, to more safely and effectively respond to 9-1-1 calls.” says Michael Redlener, the President of the NEMSQA Board of Directors.
“By utilizing less lights and sirens during EMS response and transport, our efforts have shown measurable increases in safety. The EMS community and the general public will surely benefit from the now-proven tactics provided by this partnership,” added Mike Taigman, Improvement Guide with FirstWatch and faculty leading the collaborative.
More about the Collaborative and participating agencies can be found in the change package and on the NEMSQA website.
The National EMS Quality Alliance (NEMSQA) is the nation’s leader in the development and endorsement of evidence-based quality measures for EMS. Formed in 2019, NEMSQA is an independent non-profit organization comprised of stakeholders from national EMS organizations, federal agencies, EMS system leaders and providers, EMS quality improvement and data experts as well as those who support prehospital care with the goal to improve EMS systems of care, patient outcomes, provider safety and well-being on a national level.
NEMSQA
Sheree Murphy
smurphy@nemsqa.org
315-396-4725
The US Fire Administration (USFA) and Fire Safety Research Institute (FSRI) have announced the commencement of a national engagement period for the National Emergency Response Information System (NERIS) Draft Data Framework. This period will end on January 19, 2024.
The EMS community is invited to offer feedback on the Draft Core NERIS Data Framework, which includes essential data schemas crucial for NERIS operations, designed to provide the EMS and fire community with the necessary data and tools for improved decision-making and enhanced incident preparedness. These schemas include:
Access the Draft NERIS Data Framework and submit feedback by January 19, 2024. To submit feedback, access the feedback submission form below after reviewing the Framework.
|
For accessibility requests or further assistance, please contact NERIS@ul.org.
Please either or Join!
Individuals with private health insurance can receive “surprise bills” for the difference between what a provider charged and what their insurance paid.
A 2021 law prohibits surprise billing for some services, and directed the Departments of Health and Human Services, Labor, and Treasury to give providers and insurers a forum to resolve disputes about how much insurers should pay for out-of-network care.
But the rollout has been challenging. As of June 2023, over 490,000 disputes have been submitted, a much larger number than anticipated by the agencies.
And 61% of the disputes are unresolved as of June 2023.
The No Surprises Act directed the departments of Health and Human Services (HHS), Labor, and Treasury to establish a federal independent dispute resolution process. The process, which was effective April 2022, is a voluntary forum for health care providers and health insurance issuers to resolve disputes about how much should be paid for out-of-network care. The payment determinations are made by certified dispute resolution entities, which serve as arbiters. The Centers for Medicare & Medicaid Services (CMS)—an agency within HHS—administers the independent dispute resolution process.
The three departments reported that parties submitted nearly 490,000 disputes from April 2022 through June 2023. About 61 percent of these disputes remained unresolved as of June 2023. According to officials from the departments, a primary cause of the large number of unresolved disputes is the complexity of determining whether disputes are eligible for the process.
Number of Out-of-Network Disputes in the Federal Independent Dispute Resolution Process by Calendar Quarter, April 15, 2022—June 30, 2023
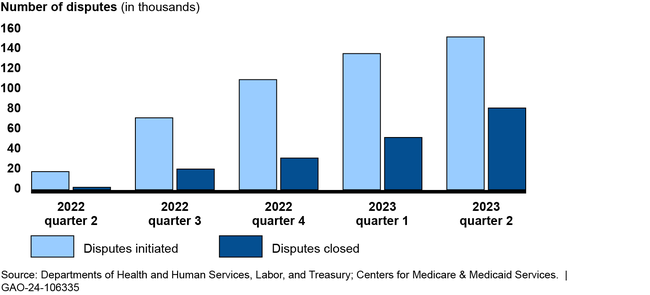
The groups GAO interviewed described a challenging roll out of the independent dispute resolution process, including a higher-than-expected dispute volume. For example, the departments anticipated about 22,000 disputes in 2022, but received nearly 490,000 through June 2023. Four groups told GAO the departments did not account for the experience of states with similar processes when making the estimate. Disputing parties and certified entities also described the broader effects of those challenges, such as backlogs resulting in delays in payment determinations. The departments have taken some actions to address challenges, such as conducting pre-eligibility reviews on submitted disputes.
To address concerns from insurers and providers, CMS and Labor look into complaints; however, stakeholder groups expressed concern with what they describe as a lack of response to submitted complaints. The departments reported limited ability to increase enforcement efforts due to budget constraints. HHS has requested a budget increase for the process, and the departments are revisiting the administrative fee amount, which is intended to cover the costs of the process, and plan to issue updated program rules.
About two thirds of individuals in the United States receive their health coverage through private health plans. Balance billing is when insured patients receive a bill from a health care provider for the difference between the amount charged and the payment received from the health insurance issuer. An unexpected balance bill is referred to as a “surprise bill” and may create a financial strain for patients. For individuals with private health insurance, the No Surprises Act prohibits providers from balance billing in certain circumstances and directed the three departments to establish the federal independent dispute resolution process.
The Consolidated Appropriations Act, 2021, includes a provision for GAO to review the federal independent dispute resolution process. This report describes (1) the number and types of disputes submitted between April 2022 and June 2023, and the status of their resolution; (2) selected stakeholders’ experiences with the process, and agency actions to address challenges; and (3) how federal agencies oversee the process.
GAO reviewed published reports, relevant federal laws, regulations, and guidance; and interviewed officials from CMS and Labor. GAO also interviewed five selected health care providers or their representatives, which accounted for nearly half of all submitted disputes as of December 2022. In addition, GAO interviewed three issuers, three certified entities that arbitrate the disputes, and 10 stakeholder groups.
For more information, contact John E. Dicken at (202) 512-7114 or dickenj@gao.gov.
NHTSA published a request for information on October 13, 2023, seeking comments from all sources (public, private, government, academic, professional, public interest groups, and other interested parties) on the planned re-envisioning of the 2000 EMS Education Agenda for the Future: A Systems Approach. Due to the limited comments received and some informal feedback indicating that the initial comment period was too short, NHTSA is announcing the reopening of the comment period for the RFI in order to solicit additional comments and request responses to specific questions provided in the document. The comment period for the RFI was originally scheduled to end on October 31, 2023. It will now be reopened and will end on March 31, 2024.
The comment period for the RFI published on October 13, 2023 at 88 FR 71081 is reopened and extended to March 31, 2024.
Clary Mole, EMS Specialist, National Highway Traffic Safety Administration, U.S. Department of Transportation is available by phone at (202) 868–3275 or by email at Clary.Mole@dot.gov.
Comments must be submitted by one of the following methods:
• Federal eRulemaking Portal: go to http://www.regulations.gov. Follow the online instructions for submitting comments.
• Mail: Docket Management Facility, M–30, U.S. Department of Transportation, West Building, Ground Floor, Rm. W12–140, 1200 New Jersey Avenue SE, Washington, DC 20590.
• Hand Delivery or Courier: West Building Ground Floor, Room W12–140, 1200 New Jersey Avenue SE, between 9 a.m. and 5 p.m. Eastern Time, Monday through Friday, except Federal holidays. To be sure someone is there to help you, please call (202) 366–9322 before coming.
Regardless of how you submit your comments, you must include the docket number identified in the heading of this document.
Note that all comments received, including any personal information provided, will be posted without change to http://www.regulations.gov. Please see the “Privacy Act” heading below.
You may call the Docket Management Facility at (202) 366–9322. For access to the docket to read background documents or comments received, go to http://www.regulations.gov or the street address listed above. We will continue to file relevant information in the docket as it becomes available. To be sure someone is there to help you, please call (202) 366–9322 before coming. We will continue to file relevant information in the Docket as it becomes available.
Privacy Act: In accordance with 5 U.S.C. 553(c), DOT solicits comments from the public to inform its decision-making process. DOT posts these comments, without edit, including any personal information the commenter provides, to http://www.regulations.gov, as described in the system of records notice (DOT/ALL–14 FDMS), which can be reviewed at https://www.transportation.gov/privacy. Anyone is able to search the electronic form of all comments received into any of our dockets by the name of the individual submitting the comment (or signing the comment, if submitted on behalf of an association, business, labor union, etc.). You may review DOT’s complete Privacy Act Statement in the Federal Register published on April 11, 2000 ( 65 FR 19477–78 ).
On October 13, 2023, NHTSA published a RFI to obtain public comments to inform EMS Education Agenda 2050, and request responses to specific questions provided in this document. For convenience purposes, NHTSA is republishing introductory information, background materials and questions from its RFI in this notice.
In 2012, the National EMS Advisory Council (NEMSAC) convened a national roundtable meeting on EMS Education Agenda for the Future: A Systems Approach. In a 2014 report on these proceedings, NEMSAC advised that stakeholders at the State and local level had just begun to experience the full impact of the evolution toward a national integrated system of education for EMS personnel. While stakeholders were reticent to move forward with a new education agenda, they did provide feedback about themes that should be considered in the future publication. From the feedback collected at the meeting, NEMSAC developed recommendations to be used in the eventual re-envision of the agenda for EMS. These recommendations are summarized below:
• Mobile Integrated Healthcare has received considerable attention from the EMS Community. This and other alternative community-based healthcare delivery models (of the future) should evoke an expanded foundational knowledge and critical thinking capabilities that will poise future EMS practitioners to be able to evolve with the changing healthcare system or rapidly adjust to emerging healthcare crises.
In the 10 years since NEMSAC’s roundtable meeting, the national EMS education system continued to evolve—especially during the COVID–19 pandemic. In late 2021, the Federal Interagency Committee on EMS (FICEMS) began sponsoring listening sessions to inform a consensus-driven, national report entitled, FICEMS: EMS and 911 COVID–19 Response White Paper. This publication cited challenges and solutions collected during stakeholder listening sessions for the EMS education system. Among the challenges, EMS education stakeholders cited scarcity (in some cases deficits) in resources for education, rigidity of curriculum delivery modalities, the increased employer demands on students, and inconsistent or delayed responses to the needs of the national EMS education system as major contributors that led to the breakdown in the EMS workforce pipeline.
Prior to the COVID–19 pandemic, NHTSA published EMS Agenda 2050: A People-centered Vision for the Future of EMS (Agenda 2050). This collaborative project set a vision for a people-centered EMS systems that serves every individual in every community across the Nation. Later this year, NHTSA and its partners will begin a new project to develop EMS Education Agenda 2050. This project will not replace but build upon the achievements of the 2000 EMS Education Agenda for the Future: A Systems Approach to lead a national conversation around the future vision for EMS Education and EMS as a profession.
NHTSA, in partnership with Health Resources and Services Administration, published EMS Education Agenda for the Future: A Systems Approach ( Education Agenda ) in 2000. This document was founded on the broad national EMS education system concepts introduced in the EMS Agenda for the Future (1996). The Education Agenda described a consensus vision of an EMS education system with a high degree of structure, coordination, and interdependence. It proposed a less prescriptive system that offered educators flexibility in creating a student-centered learning environment and a process for accommodating future advancements in technology and medicine. The proposed system maximized efficiency, consistency in instructional quality, and entry level graduate competency by prescribing a high degree of structure, coordination, and interdependence. To achieve this vision, the education system of the future centered on five integrated primary components:
After the Education Agenda was published, stakeholders began implementing their respective integrated system components. Almost 25 years later, the national EMS education system has successfully evolved into one that exemplifies both consistency and flexibility. System interdependencies have helped to avoid duplication of effort in curriculum and education program development, evaluating the minimum competencies of graduates, certification and licensing processes, and facilitation of practitioner reciprocity.
In 2020, the EMS education system interdependencies modernized by the Education Agenda were tested. Challenges presented by the COVID–19 pandemic forced a variety of adaptations. Traditional education programs reported a lag in students’ capabilities of achieving the programmatic competencies requirements for graduation. The lag was attributed to a variety of causes including a focus on pandemic response activities over training and education, employer demands on working students, and the rigidity of in-person, classroom-based education delivery models. After the majority of programs adjusted to the challenges, lags in graduation were cured, and students achieved programmatic competencies at rates similar to those pre-pandemic. The response to the pandemic did not impact education programs only. The impact to EMS agency daily operations was felt as well. During the COVID pandemic, agencies experienced increases in EMS activation and response rates which created additional stressors for student EMS practitioners already working in a high stress job environment but also enrolled in an EMS education program. These stressors were a major contributor to a migration of practitioners away from the EMS workforce. Agencies and organizational stakeholders asserted that it could be education program graduation requirements causing breakdown in the workforce pipeline; however, there were no observed decreases in graduation or certification testing rates. These observations prompt two questions: If graduation and certification testing rates have remained unchanged, why have agencies reported recruitment and retention issues? If graduates are not entering the EMS workforce, where are they finding jobs?
With agencies experiencing increased demand and a deficiency in qualified EMS practitioners to respond to it, service delivery models had to evolve. To bridge the gap in community-based care resources, community paramedicine and mobile integrated healthcare (CP–MIH) service delivery models increased in prevalence, and improvised training programs were used to close new job-specific competency gaps among existing EMS practitioners and individuals in training. Other themes brought to the forefront during the pandemic include addressing healthcare disparities; the use of EMS data as a tool for surveillance and nationwide quality of care improvements; and a greater value to having an EMS workforce that is not only equitable, inclusive, and accessible, but as diverse as the community it serves. These themes, evolving service delivery models, and the subsequent evolution of competencies needed by practitioners suggest that it is time for NHTSA to gather our partners to begin a new conversation about the future of EMS Education and EMS as a profession in the United States.
Responses to the following questions are requested to help plan the revision of the Education Agenda. Please be as specific as possible and as appropriate please provide references.
1. What are the most critical issues facing EMS education system that should be addressed in the revision of the EMS Education Agenda ? Please provide specific examples.
2. What progress has been made in implementing the EMS Education Agenda since 2000?
3. How have you used EMS Education Agenda ? Please provide specific examples.
4. As an EMS Stakeholder, how might a revised EMS Education Agenda be most useful to you?
5. What significant changes have occurred in the EMS education system at the national, Federal, State, and local levels since 2000?
6. What significant changes will impact the EMS education system in the next 25 years?
7. How might the revised EMS Education Agenda contribute to enhanced EMS for children?
8. How might the revised EMS Education Agenda support and/or promote data-driven and evidence-based improvements in EMS education systems and EMS practitioner practice?
9. How could the revised EMS Education Agenda enhance collaboration among EMS systems, health care providers and facilities, public safety answering points, public health, public safety, emergency management, insurers, and others?
10. How could the revised EMS Education Agenda be used to promote community sustainability and resilience?
11. How could the revised EMS Education Agenda contribute to improved coordination for disaster response, recovery, preparedness, and mitigation?
12. How could the revised EMS Education Agenda enhance the exchange of evidence-based practices between national, Federal (and military), State, and local levels?
13. How could the revised EMS Education Agenda support the seamless and unimpeded transfer of military EMS personnel to roles as civilian EMS providers?
14. How could the revised EMS Education Agenda support interstate credentialing of EMS personnel?
15. How could the revised EMS Education Agenda support improved patient outcomes in rural and frontier communities?
16. How could the revised EMS Education Agenda lead to improved EMS systems in tribal communities?
17. How could the revised EMS Education Agenda promote a culture of safety among EMS personnel, agencies, and organizations?
18. Are there additional EMS attributes that should be included in the revised EMS Education Agenda ? If so, please provide an explanation for why these additional EMS attributes should be included.
19. Are there EMS attributes in the 2000 EMS Education Agenda that should be eliminated from the revised edition? If so, please provide an explanation for why these EMS attributes should be eliminated.
20. What are your suggestions for the process that should be used in revising the EMS Education Agenda ?
21. What specific agencies/organizations/entities are essential to involve, in a revision of the EMS Education Agenda ?
22. Do you have any additional comments regarding the revision of the EMS Education Agenda ?
(Authority: 23 U.S.C. 403(b)(1)(A)(iv); 49 CFR 1.95; 501.8)
Issued in Washington, DC.
Please either or Join!